New Cholesterol-Lowering Pill Shows Promise for High-Risk Heart Patients
A Breakthrough in Cardiovascular Medicine
Medical researchers have unveiled exciting news for millions of Americans struggling with high cholesterol despite current treatments. A groundbreaking experimental pill called enlicitide has demonstrated remarkable effectiveness in reducing dangerous cholesterol levels in people who remain at significant risk for heart attacks even while taking standard statin medications. This development could represent a major leap forward in how we manage one of the nation’s most serious health threats. The research, published in the prestigious New England Journal of Medicine, involved nearly 3,000 high-risk patients and showed that this new medication could slash LDL cholesterol—the harmful kind that clogs arteries—by an impressive 60% over a six-month period. What makes this particularly noteworthy is that enlicitide works through a mechanism that until now has only been available through injected medications, potentially offering a much more convenient option for patients who need extra help beyond what statins alone can provide.
Understanding the Scale of the Problem
Heart disease remains America’s number one killer, claiming more lives than any other condition. At the heart of this epidemic lies high LDL cholesterol, which causes dangerous plaque to accumulate in our arteries, setting the stage for potentially fatal heart attacks and strokes. While doctors consider an LDL level of 100 acceptable for generally healthy individuals, the bar is set much higher for those already dealing with cardiovascular issues. Medical guidelines recommend reducing LDL to at least 70 for people with high cholesterol or existing heart disease, and pushing even lower for those facing the greatest danger. This is where the challenge begins for many patients and their healthcare providers. Statin medications like Lipitor and Crestor, along with their affordable generic versions, have been the foundation of cholesterol treatment for decades and work quite effectively for many people by blocking the liver’s cholesterol production. However, even when patients max out their statin doses, a significant number still can’t bring their cholesterol down to the recommended safe levels, leaving them vulnerable to cardiovascular events despite doing everything right with their current treatment plan.
How the New Pill Stacks Up Against Current Options
The major clinical trial that tested enlicitide involved more than 2,900 patients at high risk for heart complications who were randomly divided into two groups—one receiving the experimental pill daily in addition to their regular treatment, and another getting a placebo dummy pill. Dr. Ann Marie Navar, a cardiologist at UT Southwestern Medical Center who led the study, emphasized that while other pills can be added to statin therapy, none come anywhere close to matching the dramatic LDL cholesterol reduction achieved with enlicitide. The benefits proved remarkably durable too, with only a slight decrease in effectiveness when researchers tracked patients over a full year. Equally important, the safety profile looked good—researchers found no meaningful difference in adverse events between those taking the real medication and those on the placebo. There is one practical consideration patients would need to manage: the pill must be taken on an empty stomach to work properly. This requirement might pose a minor inconvenience, but it’s likely a small price to pay for such substantial cholesterol reduction without needles.
Filling a Critical Gap in Treatment
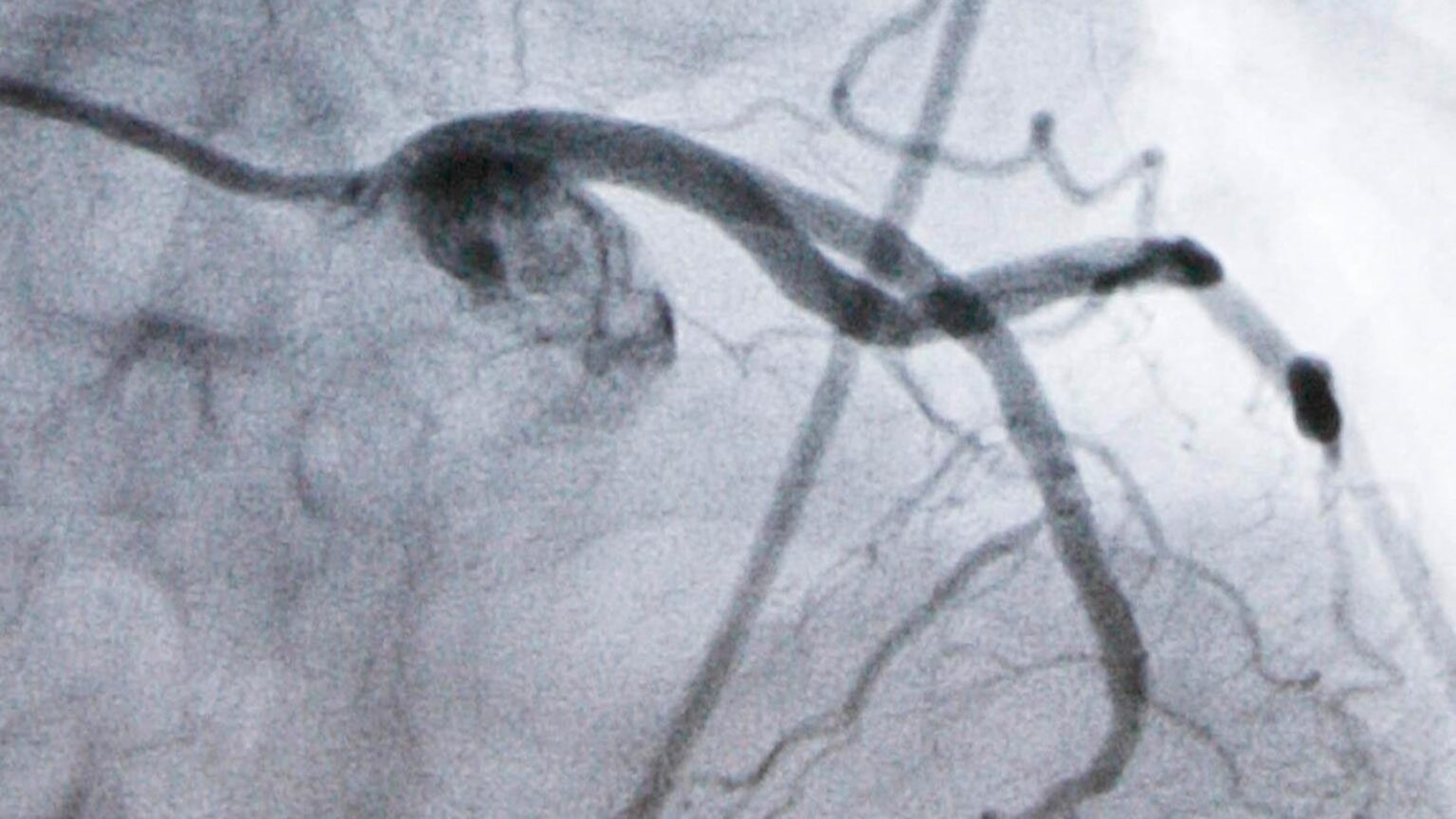
Currently, when statins alone aren’t sufficient, doctors can prescribe powerful injectable medications that work through a completely different mechanism than traditional cholesterol pills. These PCSK9 inhibitors, as they’re called, block a specific liver protein that normally limits how efficiently our bodies can clear cholesterol from the bloodstream. While highly effective, these injections have seen disappointing uptake among the population that could benefit from them. Several factors contribute to this underuse. Although prices have come down from their initially astronomical levels, the shots remain expensive for many patients and insurance systems. Beyond cost, there’s the simple reality that many people strongly dislike giving themselves shots, which creates a psychological barrier to treatment. Dr. Navar also pointed out that from the physician’s perspective, prescribing these injectable medications involves more complexity and paperwork compared to simply writing a prescription for a pill. These practical hurdles mean that countless high-risk patients who could theoretically benefit from PCSK9 inhibition simply don’t receive it, leaving a dangerous gap between what medicine can offer and what patients actually receive in real-world practice.
The Path Forward and What Questions Remain
Pharmaceutical company Merck, which funded this latest research, now has some of the critical final data needed to submit enlicitide for Food and Drug Administration approval. The regulatory outlook appears promising—the FDA has placed the drug into a special program designed to expedite review of medications that address serious unmet medical needs. Dr. William Boden from Boston University and the VA New England Healthcare System, an independent expert who wasn’t involved in the study, wrote an accompanying analysis in the journal calling the evidence “compelling” that this new pill lowers cholesterol roughly as effectively as the existing PCSK9 injection treatments. However, Dr. Boden also raised an important cautionary note that highlights the difference between surrogate markers and ultimate outcomes. While the study convincingly demonstrates that enlicitide reduces cholesterol numbers on blood tests, we don’t yet have proof that this laboratory improvement translates into what patients and doctors really care about—fewer heart attacks, fewer strokes, and people living longer, healthier lives. Establishing that connection requires following patients for much longer than the one year covered in this initial study. Understanding this limitation, Merck has already launched a much larger trial involving more than 14,000 patients specifically designed to answer these crucial questions about real-world cardiovascular outcomes.
A Promising Development in the Fight Against Heart Disease
The potential approval of enlicitide represents more than just another medication option—it could fundamentally change the treatment landscape for cardiovascular disease in America. By offering PCSK9 inhibition in pill form rather than requiring injections, this new drug could remove significant barriers that currently prevent many high-risk patients from receiving optimal treatment. The convenience factor alone could dramatically improve medication adherence, as research consistently shows that people are more likely to consistently take treatments that fit easily into their daily routines. For the millions of Americans whose cholesterol remains dangerously elevated despite their best efforts with statins, enlicitide could provide a realistic pathway to reaching safe levels and significantly reducing their risk of life-threatening cardiovascular events. While we await the longer-term outcome studies and FDA decision, the initial results certainly justify optimism. As we continue the long-standing battle against heart disease—our nation’s most lethal health threat—new weapons like enlicitide remind us that medical innovation continues to advance, offering hope for better, longer lives for patients struggling with conditions that were once considered poorly treatable.