Supreme Court Examines Challenge That Could Eliminate Free Preventive Care Under Obamacare
The Stakes of the Legal Battle
The Supreme Court is currently wrestling with a challenge that could fundamentally reshape how millions of Americans access preventive healthcare services. At the heart of this legal battle lies one of the Affordable Care Act’s most popular provisions—the requirement that insurance companies cover certain preventive health services without charging patients anything out of pocket. This seemingly straightforward benefit has become the subject of intense constitutional scrutiny, and the outcome could affect everything from annual checkups and cancer screenings to vaccinations and mental health counseling for over 150 million Americans with private insurance. Dr. Zeke Emanuel, one of the architects of the Affordable Care Act, has weighed in on the proceedings, highlighting the potentially devastating consequences if the Court sides with the challengers. The case represents yet another attempt to dismantle key components of Obamacare, more than a decade after its passage, and demonstrates how the law remains a political and legal lightning rod in American healthcare policy.
The provision in question has allowed people to receive services like mammograms, colonoscopies, blood pressure screenings, and cholesterol tests without copays or deductibles. For many Americans, particularly those living paycheck to paycheck, these no-cost preventive services have made the difference between catching diseases early when they’re most treatable and going without care altogether. Preventive medicine has long been recognized as one of the most cost-effective approaches to healthcare—catching cancer in its early stages, for instance, is far less expensive and more successful than treating advanced disease. The Affordable Care Act’s preventive care mandate was designed to remove financial barriers that might discourage people from getting the screenings and checkups they need. Now, this fundamental principle of accessible preventive care hangs in the balance as the Supreme Court considers whether the mechanism used to determine which services must be covered violates the Constitution.
Understanding the Constitutional Challenge
The legal challenge centers not on whether preventive care is valuable or whether Congress can require insurance coverage, but rather on how the specific services are selected for mandatory coverage. Under the Affordable Care Act, decisions about which preventive services must be covered without cost-sharing are made by the United States Preventive Services Task Force, an independent panel of medical experts. The challengers argue that this delegation of authority to an advisory body whose members are not appointed by the President and confirmed by the Senate violates the Appointments Clause of the Constitution. They contend that because these task force members wield significant regulatory power by determining what services insurance companies must cover, they should be considered “principal officers” of the United States and therefore subject to the constitutional requirements for appointment.
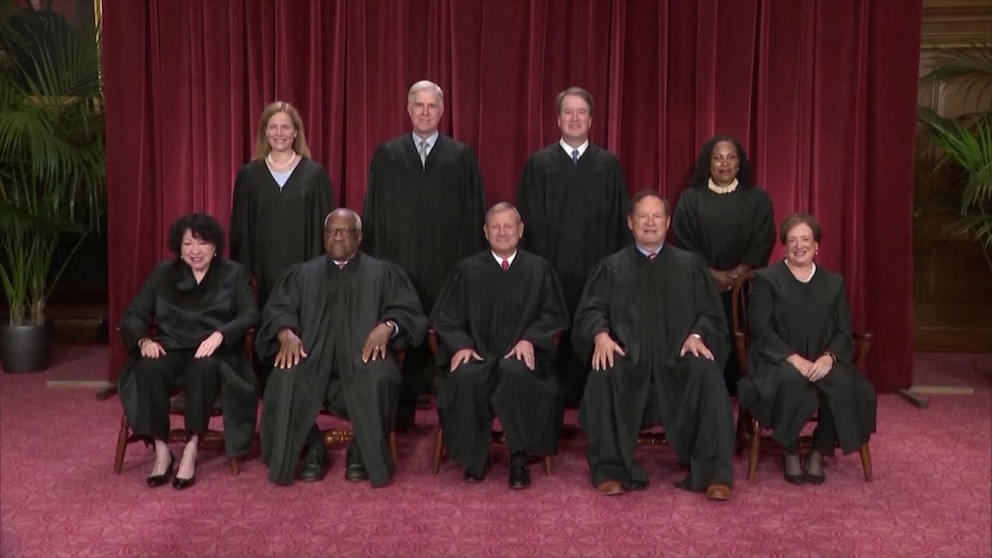
This argument may sound technical, but its implications are enormous. If the Supreme Court agrees with the challengers’ interpretation, it could invalidate not just the preventive care mandate but potentially call into question numerous other regulatory structures across the federal government that rely on expert panels and advisory bodies. The case touches on fundamental questions about the separation of powers, the administrative state, and how much authority Congress can delegate to executive branch agencies and advisory bodies. Conservative justices have increasingly shown skepticism toward what they view as the unchecked growth of administrative power, while liberal justices tend to defer more readily to agency expertise and congressional decisions about how to structure government functions. The case also reflects broader ideological battles about the proper scope of federal regulation and the role of unelected experts in policymaking.
What’s at Risk for American Patients
If the Supreme Court rules in favor of the challengers, the immediate impact on American healthcare consumers could be substantial and swift. Insurance companies might no longer be required to cover preventive services without cost-sharing, meaning patients could face copays, deductibles, or coinsurance for services they currently receive for free. For someone needing a colonoscopy, this could mean paying hundreds or even thousands of dollars out of pocket. For families relying on free vaccinations for their children or annual wellness visits, the sudden introduction of costs could force impossible choices between healthcare and other necessities like rent, groceries, or utilities. Studies have consistently shown that when financial barriers exist, people delay or forgo preventive care, leading to later diagnoses, worse health outcomes, and ultimately higher costs when conditions that could have been caught early require more intensive treatment.
Dr. Emanuel and other healthcare policy experts have emphasized that eliminating free preventive care would be particularly harmful to lower-income Americans and communities of color, who already face significant health disparities. The preventive care mandate has been especially important in addressing these inequities by ensuring that access to screenings and early intervention isn’t determined by ability to pay. Research has shown that since the Affordable Care Act’s preventive care provisions took effect, the number of people receiving recommended cancer screenings, cardiovascular assessments, and other preventive services has increased significantly. Women have particularly benefited from provisions requiring coverage of mammograms, cervical cancer screenings, and contraception without cost-sharing. Reversing these gains could set back years of progress in public health and health equity, potentially leading to more preventable deaths and suffering, particularly among vulnerable populations who are least able to afford unexpected medical expenses.
The Political and Ideological Context
This Supreme Court challenge represents the latest chapter in a long-running campaign to dismantle or weaken the Affordable Care Act, which has survived multiple existential threats since its passage in 2010. The law has been challenged in Congress, in state legislatures, and repeatedly in the courts, with opponents attacking different provisions on various legal grounds. While the Supreme Court upheld the individual mandate in 2012 and rejected another challenge to the law’s subsidies in 2015, conservatives have continued searching for vulnerabilities that might unravel the law or limit its reach. This particular challenge is notable because it doesn’t attack the entire law but focuses on a specific, popular provision, potentially making it more difficult for defenders to rally public support. After all, even many people who oppose the Affordable Care Act as a whole appreciate not having to pay for preventive care.
The case also arrives at a time when the Supreme Court’s conservative majority has shown increasing willingness to constrain federal regulatory authority and question long-standing administrative law doctrines. Recent decisions have limited the Environmental Protection Agency’s authority to regulate carbon emissions, struck down the Biden administration’s student loan forgiveness plan, and narrowed federal agencies’ ability to interpret ambiguous statutes. This trend toward limiting administrative power reflects a broader conservative legal philosophy that views the growth of the administrative state with suspicion and seeks to return more decision-making authority to Congress or to limit government power altogether. The preventive care challenge fits neatly into this framework, allowing the Court to potentially curtail federal health regulation while claiming to vindicate constitutional principles about the separation of powers rather than making a direct judgment about healthcare policy.
Dr. Emanuel’s Perspective and Broader Healthcare Implications
As one of the Affordable Care Act’s architects, Dr. Zeke Emanuel brings both technical expertise and a deep understanding of the law’s intent to the debate surrounding this challenge. Emanuel has argued that the preventive care mandate represents exactly the kind of evidence-based, cost-effective healthcare policy that should be encouraged, not dismantled. He has emphasized that the Preventive Services Task Force was deliberately designed to insulate decisions about which services to cover from political interference, ensuring that recommendations would be based on scientific evidence rather than lobbying or partisan considerations. The task force reviews medical research, assesses the effectiveness of various preventive services, and makes recommendations based on data and expert consensus—precisely the kind of rigorous, non-political decision-making that should guide healthcare policy.
Emanuel and other healthcare experts worry that beyond the immediate impact on patients’ access to preventive care, a ruling against the government could create broader uncertainty throughout the healthcare system and regulatory environment. If the Court invalidates the current structure for determining covered preventive services, it might also call into question similar expert bodies that make recommendations on everything from vaccine schedules to clinical practice guidelines. The ripple effects could extend beyond healthcare to other areas of regulation that rely on expert panels and advisory bodies. Moreover, there’s concern that even if Congress could theoretically fix the constitutional problem by restructuring how task force members are appointed, the current political dysfunction and polarization make such legislative solutions unlikely. In today’s gridlocked Congress, even broadly popular measures struggle to pass, and anything associated with Obamacare faces automatic opposition from many Republicans. The result could be a legal vacuum where the preventive care mandate is invalidated but no workable alternative is implemented, leaving insurers, healthcare providers, and patients in limbo about what services must be covered and at what cost. This uncertainty could further destabilize insurance markets and create enormous administrative challenges as companies try to adjust their coverage policies amid unclear legal requirements.